Growth and Adoption of Value-Based Care
This article is one in a series that advocates the need to bring specialty care under value-based care payment models. Click here to read the previous article, All Participants Must Come Together to Deliver the Promise of Value-Based Care.
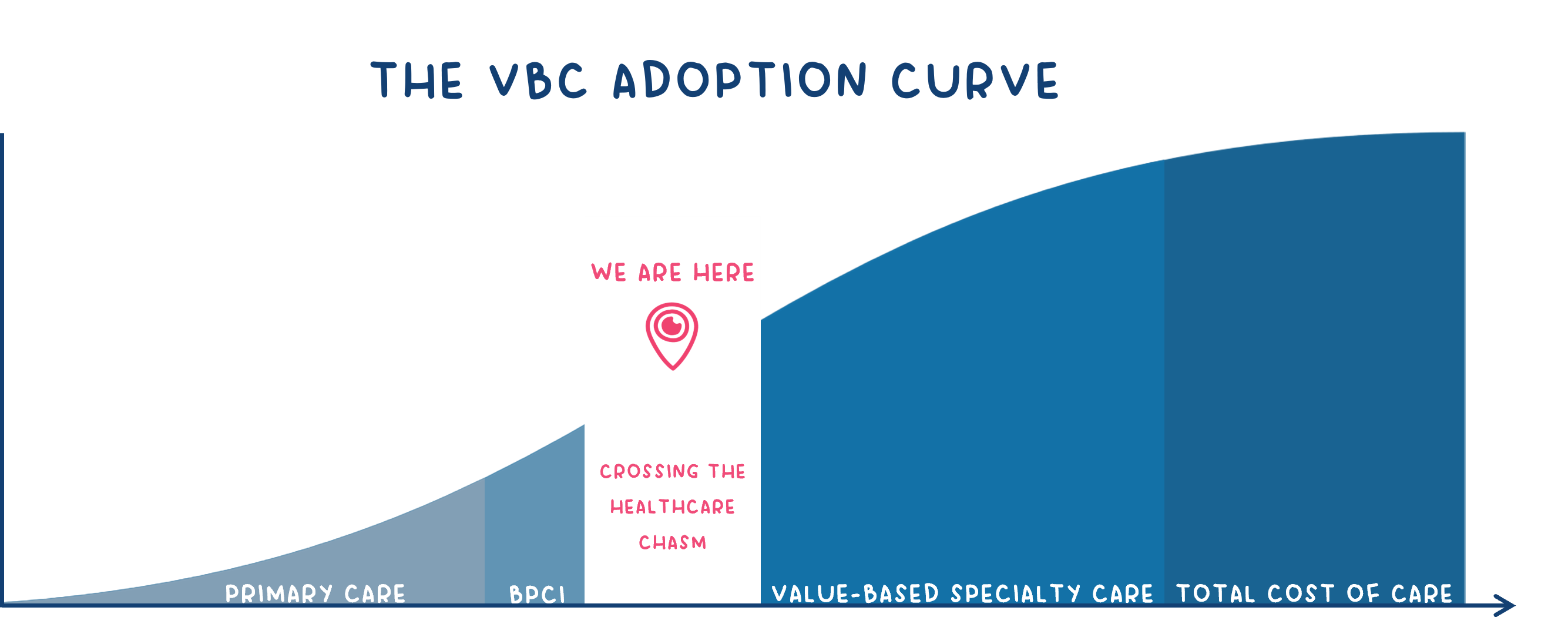
It Will Take Specialty Care to Bend the VBC Curve
Meaningful progress has been made on the road to broad success of value-based care, but predominately in the primary care sector.
Significantly less headway has occurred in specialty care.
Specialty providers represent the majority of healthcare costs in America, but for the most part, are still doing business under traditional fee-for-service payment models. Despite the promise (and proof) that value-based care works, most specialty care providers continue to be financially rewarded based on volume, rather than quality outcomes. Simply put, most of the specialty care is driven by more visits scheduled, more procedures performed, and more interventions ordered.
Conversely, primary care providers, often a patient’s first point of entry into the healthcare system, control a minority of medical costs in our country. While positive change has occurred in primary care through value-based payment models, the financial impact represents a fraction of total cost of care provided.
The question, “if value-based care is a proven approach in our healthcare system, why is specialty care not incented like primary care?”
Aligned Financial Incentives Are the Key
While primary care is focused on prevention and/or managing chronic conditions, each category of specialty care (and there are more than 135, according to the American Association of Medical Colleges) involves many unique conditions, treatments, procedures, and interventions. The complexities of specialty care make the development of value-based programs more challenging; however, it can be done. So, why hasn’t value-based care been adopted into specialty yet?
The root cause of the dysfunctional healthcare system lies in the absence of a cohesive financially aligned model that incentivizes best-in-class care over volume. Refusing to change is equivalent to preserving the existing state and anticipating a different result, which keeps all parties gripped with frustration.
Without incentives harmonized across the care continuum, the financial model is destined to fail. A model that aligns incentives and fosters the right mindset is essential to guide providers toward actions that can effectively bend the cost curve.
A Scenario That’s All Too Familiar
A patient walks in, grimacing with joint pain, hoping for relief. Receiving an injection would likely alleviate their pain; however, that patient may leave without an injection and without relief, but with a six-week physical therapy order. After six weeks of physical therapy the patient might not see significant improvement and could require an injection or, in some cases, surgery. The payer does not approve the injection or surgery immediately, as they insist on exhausting other treatments first. Why? Payer guidelines, while necessary, come with their own set of challenges. They’re crafted with a cautious approach aiming to conserve resources. While well-intentioned, this method inadvertently inflates the overall cost of care, leaving both patients and providers caught in a complex web of policies and financial incentives.
Bringing Value-Based Care into Specialty
Empowering healthcare providers is key to informed decision-making and driving improvement in patient care. In order to effectively incorporate value-based care principles into specialty care, the following steps must be taken:
- Standardizing quality and outcome metrics across the continuum
- Increasing provider access to data and digestible analytics
- Accommodating variability in specialty care conditions and treatments in VBC models
- Facilitating care coordination between primary care and specialty care providers
- Motivating the involvement of both primary care and specialty care providers through proper incentives
- Educating PCPs on proactive engagement, symptom recognition, and care administration
Education Fosters Success
Imagine a world where doctors held the power to heal but were unaware of the impact of their decisions. Ignorance of the true cost of care led to outdated orders and practices. Every joint patient would be referred to skilled nursing whether or not they needed it after surgery. This was the reality for OrthoPods prior to implementing the Bundled Payments for Care Improvement (BPCI) program with CMS. BPCI showed the patient journey and associated expenditures through a different lens giving providers timely feedback. Now instead of just relying on historical data to shape the program, real-time live feeds of claims allow these providers to pinpoint issues and pivot to adaptive strategies on a dime.
While BPCI was a good start, it had limited success. This was mainly due to lowering the targets too quickly and allowing the conveners a chance to completely change the way care was delivered. Had the financial targets been kept in place for a longer period of time, a broader shift would have been experienced. The true cost of the post-acute spend was clearly identified in this program. Surgeons were finally able to see how their patients did after surgery, as well as have a clear picture of what really occurs after the patient leaves the operating table.
Enlace is leading the charge to extend VBC to the specialty care arena. While there are challenges, there’s growing recognition of the need to put value-based care concepts at work across the entire healthcare ecosystem.
To make the impact our healthcare system needs to best serve all patients, VBC must be expanded to encompass care provided by the full range of healthcare providers.
References:
4 Ways to Improve Specialty HealthCare in the U.S.
Why Specialists Are the Next Frontier of Health Plans’ Value-Based Care Agenda
 ASK ENLACE
ASK ENLACE