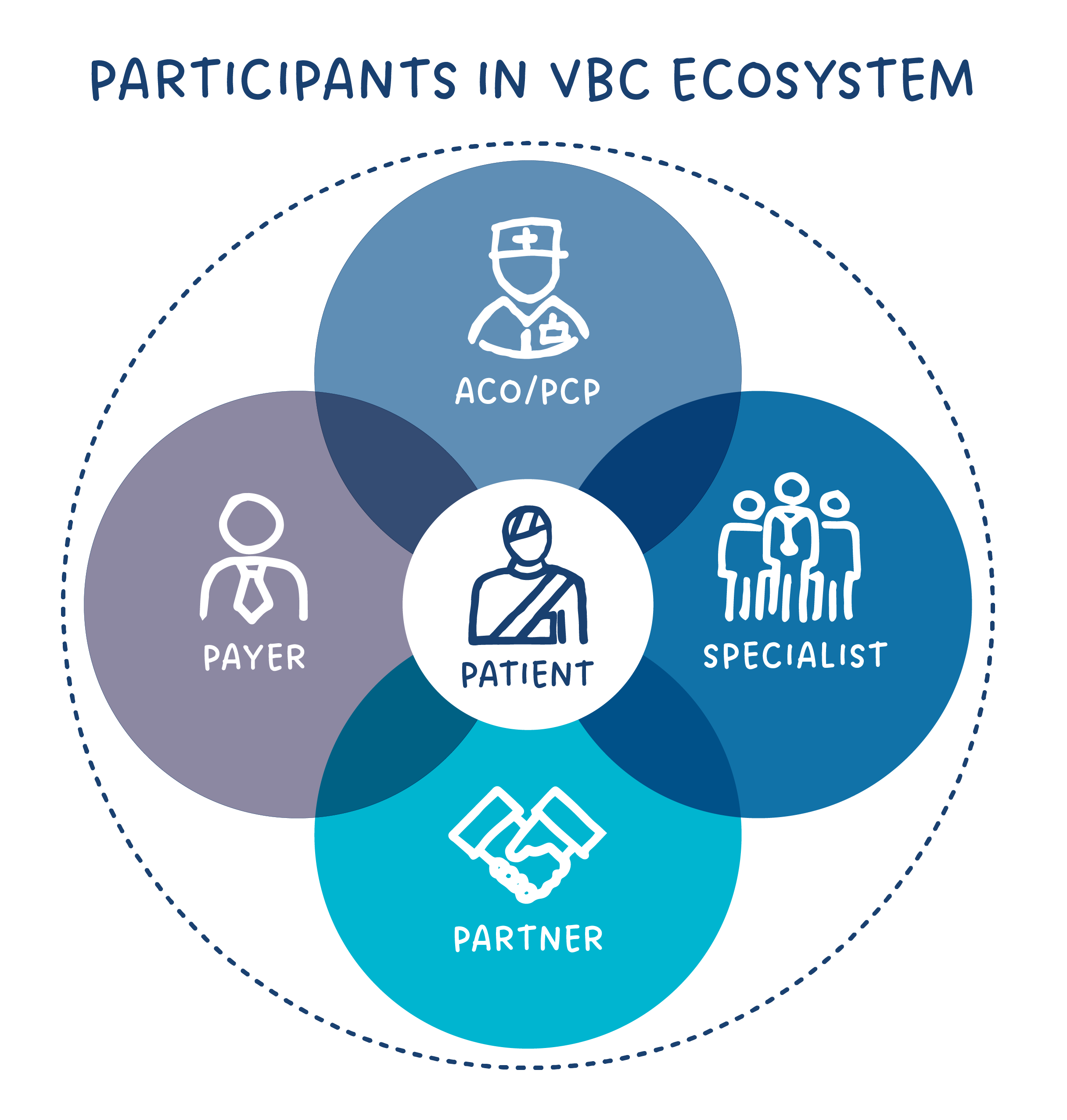
All Participants Must Come Together to Deliver the Promise of Value-Based Care
This article is one in a series that advocates the need to bring specialty care under value-based care payment models. Click here to read the previous article, VBC is Not a Do-It-Yourself Proposition.
Better care at lower cost, delivered more efficiently. That’s the goal of value-based care.
So, what does it take to build and execute successful VBC programs? What’s needed from each participant – payer, primary care, and specialty care?
Broad adoption of meaningful value-based programs requires cooperation, coordination, and aligned incentives. Despite the vast potential benefits, obstacles including legacy systems, inefficient care pathways, and misaligned incentives continue to hinder real change. Payers need to actively share financial insights and data. Primary care needs better integration throughout the entire patient journey. Specialists need to adopt value-based programs. All of these are possible within a connected system.
Each Participant Has an Essential Role to Play
Payers Need to Actively Update Financial Models and Share Data
As the foundation of the financial framework, health insurers and government payers have been tasked with designing payment models that reward positive outcomes versus volume of services.
Capitation has helped primary care shift the focus to preventive care and care coordination. Bundled payment programs, like BPCI, helped drive early value-based specialty care. However, primary care and specialty care have not seen similar integrated adoption. The result is limited change in savings across healthcare. To motivate providers, shared savings plans must be created to truly align financial incentives. Unfortunately, this is not the case right now.
Significant financial changes require new value-based payment models that are driven by data, and data sharing, across the entire continuum of care. Payers have the robust databases needed to make these value-based programs possible, but much of the data is either disconnected or not shared with the providers in ways that support growth. By effectively leveraging payer data, providers across the spectrum have the care metrics and insights needed to improve patient care and lower cost. While protection of financial and data assets is paramount to payers, this does not hinder expansion of value-based programs that create important financial changes.
Providers Need to Streamline Care and Improve Patient Access
The integration of PCPs and specialists is a critical step in value-based care program development and growth. With providers connected, patient care moves from its current disjointed, slow process to a patient journey that includes earlier diagnosis and quicker access to the correct providers. Best-in-class pathways make quality the driving force of improved patient outcomes and cost reduction.
In the integrated ecosystem, primary care physicians increase their ability to truly advocate for patients. Appointments with PCPs evolve from limited interactions to active engagements that help ensure patients gain understanding of their medical needs and faster access to the best specialist in the community.
Specialists’ participation in streamlined care is key to transforming value-based programs. With efficiencies built into the foundation of the patient journey, specialists can reallocate their time. They shift from a volume-based approach to a quality and accessibility approach that greatly impacts the patient journey.
Business Partners Support Value-Based Care
With so much complexity, it’s impossible to have all of the internal technology and knowledge needed to drive large changes. Payers, PCPs, and Specialists have different needs, only making solutions more challenging. Organizations need strong partnerships that augment current analytical capabilities and provide in-depth guidance.
Companies focused on data interoperability and analytics become key partners in an efficient value-based care system. The enormous volume of data is continuously processed and distributed to all participants through systems that provide end-to-end visibility and key metrics.
With more data, more analytics, and expanded programs, partners will serve as important guides in the expanding value-based care landscape. Payers gain support from in-depth expertise and provider organizations get back to doing what they want to do most – practice good medicine.
This article is one in a series that advocates the need to bring specialty care under value-based care payment models. Click here to read the next article, Growth and Adoption of Value-Based Care.
References:
U.S. Health Care from a Global Perspective, 2022: Accelerating Spending, Worsening Outcomes
Payers Play Crucial Role in Healthcare Quality Transparency
Collaborating to Support Better Outcomes Through Value-Based Care
 ASK ENLACE
ASK ENLACE