With VBC, Everyone Across the Value Chain Wins–Including Employers
Employers have a tough job. To make sure customers are well-served and their businesses continue to grow, they have to make a serious investment into attracting and retaining exceptional employees. In fact, the two highest costs that all employers incur are payroll and healthcare benefits—in that order.
The organizations that put people to work pay the majority of healthcare costs for the 160 million Americans who count on insurance benefits as part of their compensation. But, despite the fact that employers foot the bill, they’ve had little input in how our healthcare payment system works.
The contrasts between the predominant fee-for-service payment model (where healthcare is paid for based on the number of services provided) vs. a value-based care model (where payment for services is based on patient outcomes) is a hot topic among those making healthcare coverage decisions in the workplace now.
VBC Aligns with Quadruple Aim
Most in the industry understand that value-based care (VBC) is clearly the way to go. Philosophically VBC makes sense for employers, as well as every other party involved. Why? Its very definition aligns with the widely embraced Quadruple Aim targets, namely:
- Reduction of healthcare costs
- Improved population health
- A better patient experience
- Enhanced well being among healthcare teams
So while employers are well aware of the problems presented by the status quo—and have a firm grasp on the solution—they, like the majority of those with a stake in how the U.S. healthcare system works, aren’t yet sure how to get from here to there.
In the meantime, ninety-one percent of employers continue to foot the bill (averaging $22,000 per year per employee for family coverage) of all healthcare delivered in the U.S.—but have little ability to impact the payment process.
Working together, all stakeholders, including employers, can help make the American healthcare system better for all.
What’s it Take to Achieve the Benefits of Value-Based Care?
It takes an all-out, concerted effort to pursue the promise of value-based care. Providers and payers, joined by employers, need to do what they can, together, to:
- Unlock unrealized power of current technology, existing data, and team insights.
- Integrate and automate processes across the healthcare ecosystem.
- Move from retrospective to prospective payment approaches.
- Develop new ways to meet obstacles head on.
Everyone Needs to Be Pulling the VBC Oars
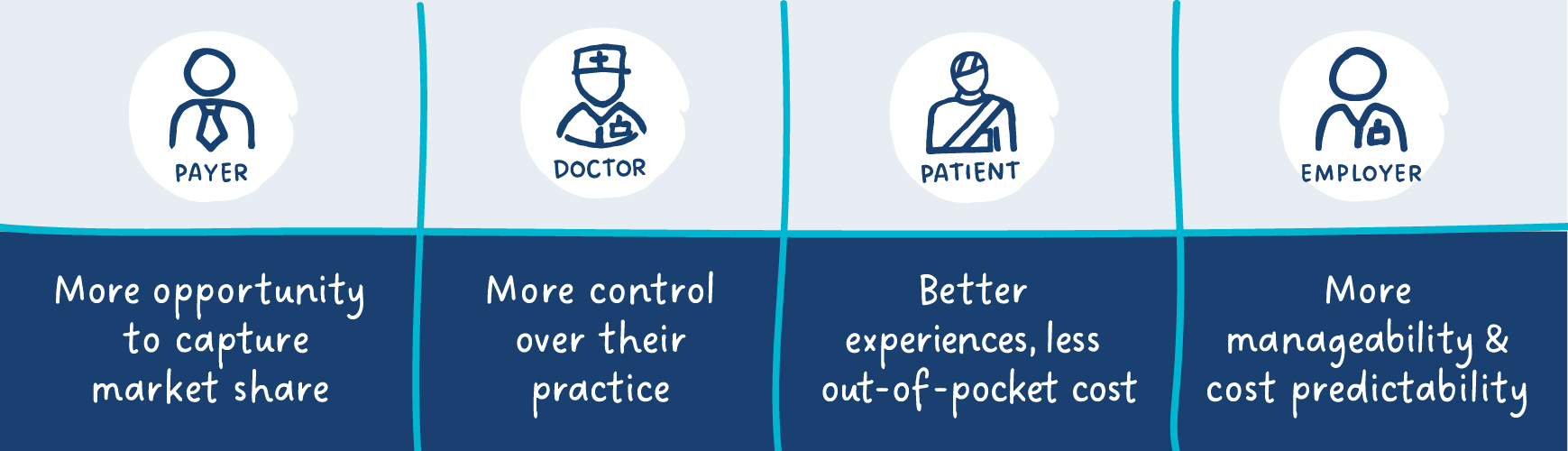
Employers must join forces with the payers, providers and patients who realize something needs to change. With a joint effort, healthcare can migrate toward a reality where, instead of pay-and-chase scenarios, excessive readmissions, surprise billings, and less-than-optimal outcomes, all are well served.
Delivering on the promise of value-based care is possible now. By automating and integrating data and processes and moving toward prospective (vs. retrospective payment approaches) the industry can overcome obstacles inherent in our current fee-for-service environment.
References:
 ASK ENLACE
ASK ENLACE