The Risk/Return Ratio of Value-Based Care is High, But Progress is Slow
This article is one in a series that advocates the need to bring specialty care under value-based care payment models. Click here to read the previous article, Changing the Healthcare Cost Trajectory Through Specialty Care.
When it comes to value-based care, most people agree it involves changing everything about how healthcare is delivered in this country. The majority also agree that that’s not a simple proposition.
Flipping our traditional fee-for-service payment model, which pays based on volume of services provided, to a value-based care payment model, which pays based on patient outcomes achieved, has been and continues to be a complex undertaking.
The term Value-Based Care has been around since 2006 when Michael Porter and Elizabeth Olmsted Teisberg coined it in their book Redefining Health Care. The authors opined that “If all (healthcare) system participants have to compete on value, value will improve dramatically.”
While VBC is a common-sense premise, it hasn’t yet had the impact it should: Healthcare costs in the U.S. have continued to rise, and quality is still not being addressed as it should.
Efforts to link care cost and care quality have had limited success, despite efforts by CMS, BCBS of Massachusetts’ Alternative Quality Contract (AQC), and the ACA, including the Center for Medicare and Medicaid Innovation (CMMI) that came on the scene in 2010, and others. Their collective endeavors to link cost and quality have not experienced the as-hoped-for impact, and an immense amount of work has yet to be done.
Issues surrounding data interoperability, care coordination, and provider alignment continue to challenge the ability to bring value-based care into the mainstream—as does the limited adoption of VBC by specialty practitioners. Only 10% of specialists participate in VBC programs, compared to 90% of primary care practitioners. This is a gap that must be closed before the promise of value-based care can be realized.
The U.S. spends far more of its GDP on healthcare than all other countries, yet its healthcare track record continues to lag, according to a recent article in the Commonwealth Fund. Among high-income countries, the U.S. has the highest rate of infant death and the highest rate of preventable deaths. Care access inequality also remains an issue, with low-income people and those in minority groups most likely to experience adverse healthcare outcomes.
America has conquered an array of difficult healthcare challenges across history. Life-saving vaccines, antibiotics, and antiviral drugs have been developed. Anesthesia, imaging, organ transplants, stem-cell therapy, and immunotherapy have altered the healthcare landscape significantly. And most recently, artificial intelligence has given us the foundation to accelerate healthcare’s pace of change for the good.
The Enlace Health team wholeheartedly believes that VBC is an endeavor with as much or more potential to make a difference in healthcare as the innovations mentioned above. Many leading healthcare industry executives and practitioners believe VBC holds the key to achieving a far more efficient, effective healthcare system than we’ve ever had before.
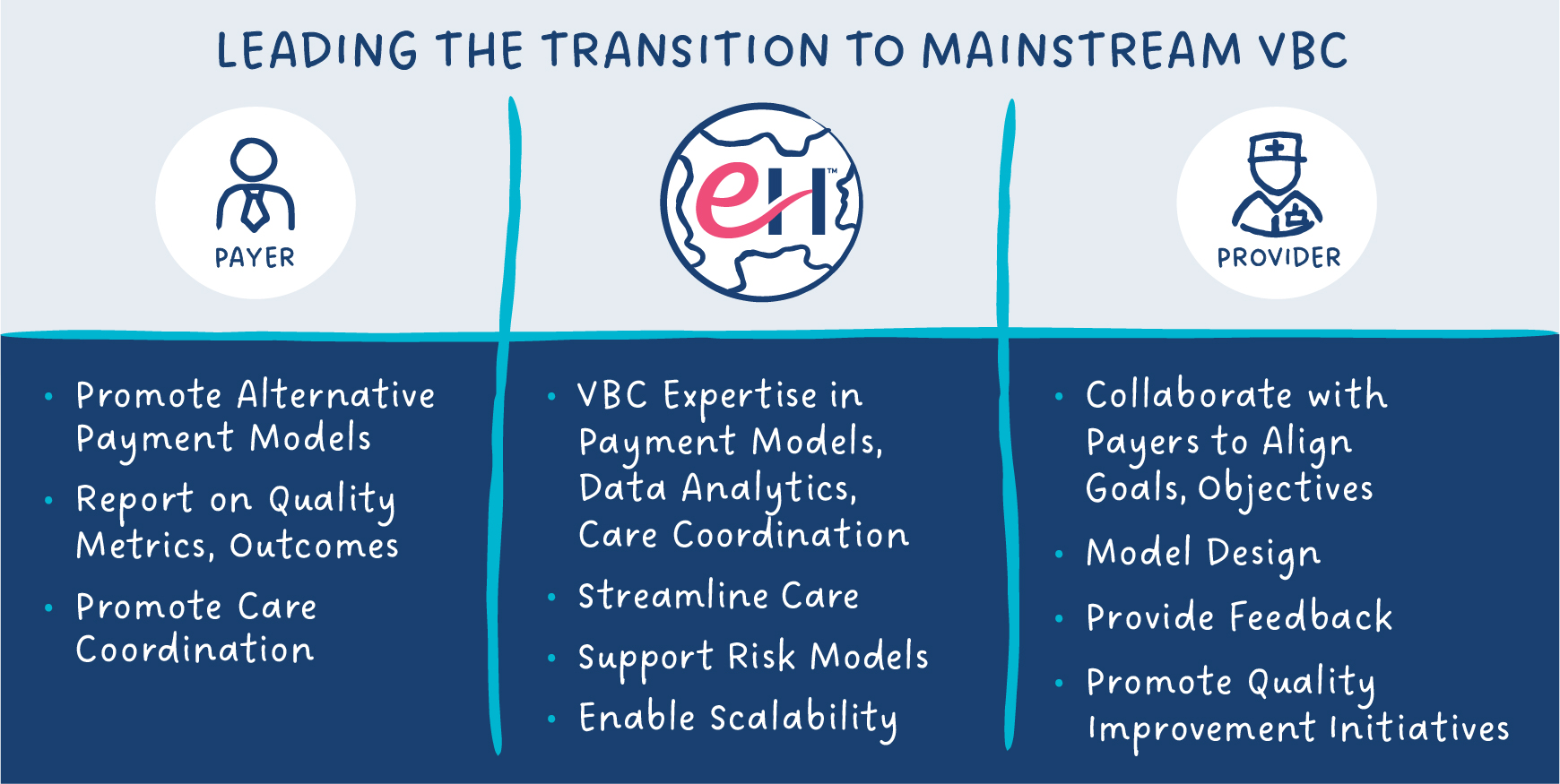
Increasingly these leaders are looking to Enlace Health as the catalyst to making value-based care a reality, benefiting providers, payers–and the patients they serve.
This article is one in a series that advocates the need to bring specialty care under value-based care payment models. Click here to read the next article, Factoring in Social Determinants of Health (SDOH): A Value-Based Care Imperative.
References:
The “Risk” of Value-Based Care
Value-Based Care: What It Is, and Why It’s Needed
 ASK ENLACE
ASK ENLACE