Fixing the U.S. Healthcare System: Government Needs to Push the Private Sector
This article is one in a series that advocates the need to bring specialty care under value-based care payment models. Click here to read the previous article, So Why Is Value-Based Care Not More Widely Embraced? If It Were Easy, Everyone Would Do It.
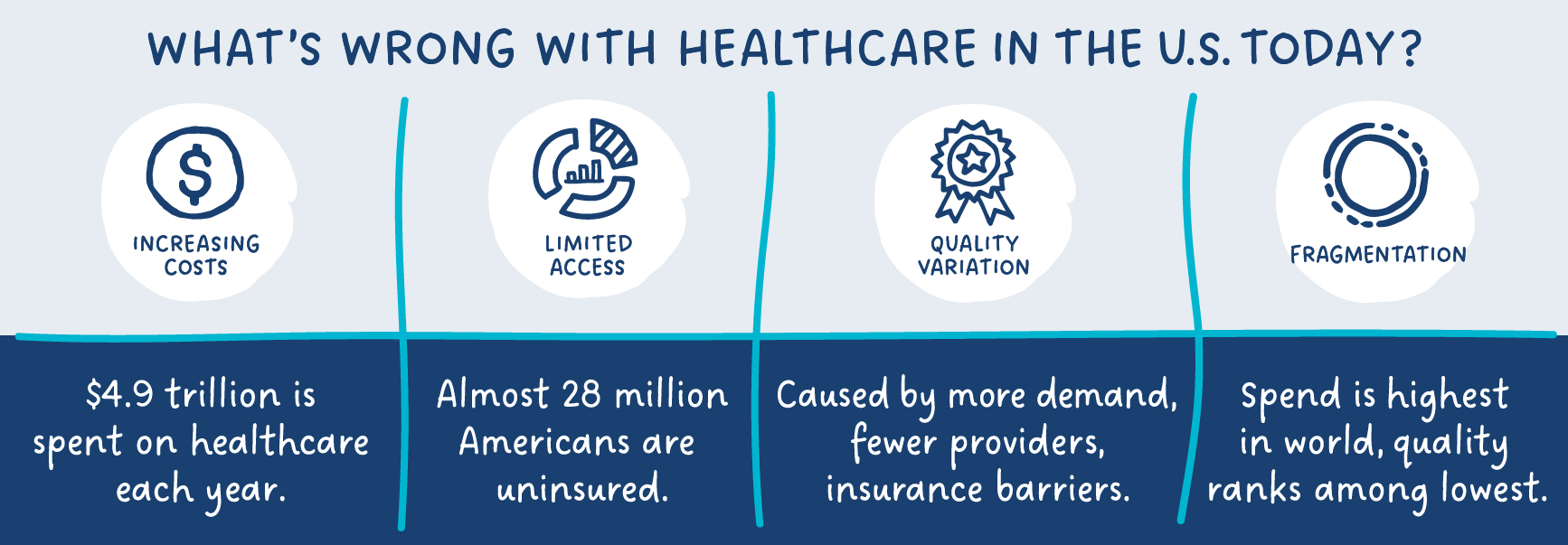
There are big problems with the way healthcare works in our country today—and that’s not news to anyone. Despite the efforts of the ACA and CMS, our care system continues to hobble along in a mostly broken state.
Unlike in other industries, when it comes to healthcare, market forces aren’t working for a large percentage of Americans. The wrong incentives are in place, and insufficient access to data impedes progress.
From an incentive standpoint, providers are paid not based on outcomes achieved but on the number of services delivered. Our traditional fee-for-service payment model rewards care quantity, not quality. That’s a fundamental flaw in our system, and it’s holding us back.
The lack of shared access to data is also keeping us from moving forward. When information isn’t able to be accessed across provider/payer organizations, it’s not possible to measure and evaluate the value of care delivered by various interventions or providers. Tracking data lets us analyze the vital metrics needed to improve access and optimize care.
So, should the government take over?
While a significant percentage of Americans support a single-payer approach (31%), according to the Pew Research Center, most don’t. The majority wants the government to influence, intervene to an appropriate extent … but not take over.
Almost 70% of us believe a balanced approach that encourages competition will drive innovation—including innovation around data transparency, outcomes, cost, and access. They believe the federal government’s role is to introduce enabling concepts that in turn support future, free-market efforts to improve our system.
Here’s an analogy that works: In the 1960s and 1970s, NASA’s efforts set the stage for future private space exploration, including SpaceX. Creating a government agency in 1958 with the goal of gathering scientific data about Earth launched a promising chain of events, as well as the space race. Now with private competitive forces at play, giant steps are being taken to advance our ability to learn more about the universe, and perhaps harness its power for the benefit of mankind.
The resulting mandates and public programs in the space case demonstrate how government action can encourage change in the right direction. Our government has the power to set the stage that encourages private entities to make positive change—in healthcare’s case, to deliver the benefits of VBC across the board.
Right now, payers and providers are approaching VBC from different angles. Clear direction as multiple parties work to make VBC work for everyone, must come from government sources.
Leading VBC innovator Enlace, and its clients, recognize this. It’s clear that nationalized healthcare isn’t the way to rectify the cost, quality, access, and fragmentation issues we’re dealing with now. But it’s equally apparent that the status quo, fee-for-service care is an approach that isn’t working. Value-based care, with compelling proof-of-concept achieved to date, holds the key.
Progress to date:
- By 2030, the Centers for Medicare & Medicaid Services’ (CMS) goal is to have all traditional Medicare recipients enrolled in value-based payment plans for specialty care. Currently, specialty-care providers provide 90% of healthcare services, but only 10% of them participate in VBC plans, according to an article in the Harvard Business Review.
This is the type of government incentive needed to bring VBC into the mainstream, and to benefit all. - The Bundled Payments for Care Improvement (BPCI) Advanced Model launched by CMS as an optional program in 2018 holds participating providers accountable for 90-day windows of care. The agency recently extended the program through 2025, as well as expanded its scope to include bundled payments for oncology care.
Government-enabled bundled payments align accountability across the care team, incenting providers, physicians, and other practitioners to work together to improve outcomes and lower costs.
Healthcare in America is complex and chaotic. Cost, access, quality, and fragmentation remain significant challenges. The government can play an essential role in creating a more orderly system. But enabling value-based care (VBC), our government can make it possible for payers, providers, and patients to participate together in a quality-driven and economically sound healthcare ecosystem.
This article is one in a series that advocates the need to bring specialty care under value-based care payment models. Click here to read the next article, Changing the Healthcare Cost Trajectory Through Specialty Care.
References:
Most continue to say ensuring health care coverage is government’s responsibility
CMS Innovation Center: Specialist Incentives for Value-Based Care
CMMI wants every Medicare beneficiary in an accountable care plan by 2030
4 Ways to Improve Specialty Health Care in the U.S.
Bundled Payments for Care Improvement (BPCI) Initiative: General Information
 ASK ENLACE
ASK ENLACE